
SC Birth Outcomes Initiative
About the Data

About the Data
The delivery hospitalization included the patient's UB-04 record with the delivery flag and any hospitalization records within 0-1 day.
They were also not flagged as the unique delivery record if occurring less than 7 months away from the previous delivery record or having the below DRGs identifying false labor, threatened abortion, antepartum admission, or postpartum admission:

Labor & Delivery
Total C-Section: Percent of total deliveries identified as cesarean on the birth record or via APR-DRG, MS-DRG, or ICD-10-PCS codes.
Total Primary C-Section: Percent of deliveries without a prior cesarean identified as cesarean on the birth record or via APR-DRG, MS-DRG, or ICD-10-PCS codes.
Primary C-Section (TJC PC-02, NTSV): This Joint Commission PC-02 Cesarean Birth Measure reflects cesareans identified by ICD-10-PCS codes (Appendix A, Table 11.06, v2025A1) among deliveries limited to gestation at least 37 weeks, first-time delivery (nulliparous), singleton, ages 10 to 64, and excluding multiple gestations and other presentations (Appendix A, Table 11.09, v2025A1).
Primary C-Section (TJC PC-02, NTSV) among patients with Cardiac Conditions in Obstetric Care : The rate of PC-02 Cesarean births among people with cardiac conditions at time of delivery. Such cardiac conditions may include congenital heart disease, cardiac valve disorders, cardiomyopathies, arrhythmias, coronary artery disease, pulmonary hypertension, and aortic dissection.
Births
Birthweight
Gestational Age
Unexpected Complications in Term Newborns (TJC PC-06, v2025A1) - Overall Rate
This measure reflects adverse outcomes in full-term newborns without pre-existing conditions. The Joint Commission uses PC-06 as a quality metric for obstetric care. The overall PC-06 rate consists of severe complications like neonatal death, birth injuries, neurological damage, and transfers to higher levels of care, as well as moderate complications or infections with longer stays. The measure is helpful to examine when interpreting rates of potentially avoidable primary cesarean (TJC PC-02).

Maternal Safety
Severe maternal morbidity (SMM) refers to life-threatening outcomes of labor and delivery. UB-04 all-payer billing data were used to calculate delivery-related SMM using ICD-10 codes associated with 20 SMM conditions, such as heart failure, renal failure, sepsis, shock, embolism, and respiratory ventilation.
This measure is then calculated for four delivery subpopulations:
Maternal Hemorrhage was identified if any of the following were present at the time of delivery:
Severe Hypertension/Preeclampsia accounts for obstetric patients with a diagnosis code for:
Cardiac Conditions in Obstetric Care (CCOC) were identified if any of the following diagnosis codes were present at the time of delivery:
Perinatal Mental Health Conditions (PMHC) refer to mood, anxiety, and anxiety-related disorders and may be inclusive of mental health conditions with onset that predates pregnancy. Note: For the dashboard, PMHC diagnoses were captured from emergency department visits or inpatient stays from one year prior to through one year after delivery, which varies from other AIM measures captured only at the time of inpatient delivery. Excluded from the AIM definition were diagnoses for substance use disorder, suicidal ideation, disruptive and conduct disorders, personality disorders, or general mental health.
The 03/27/2024 AIM Data Collection Plan and 05/14/2024 AIM SMM Codes List were used to calculate these outcomes.
Note: Given inconsistent coding of transfusions at the hospital level after the implementation of ICD-10 and less risk of maternal mortality for transfusion-only patients, as of October 1, 2022, these measures are no longer reported for patients whose only indicant of SMM was a transfusion. This will result in a decrease of SMM rates statewide.
More information about the AIM initiative can be found here: What is AIM?

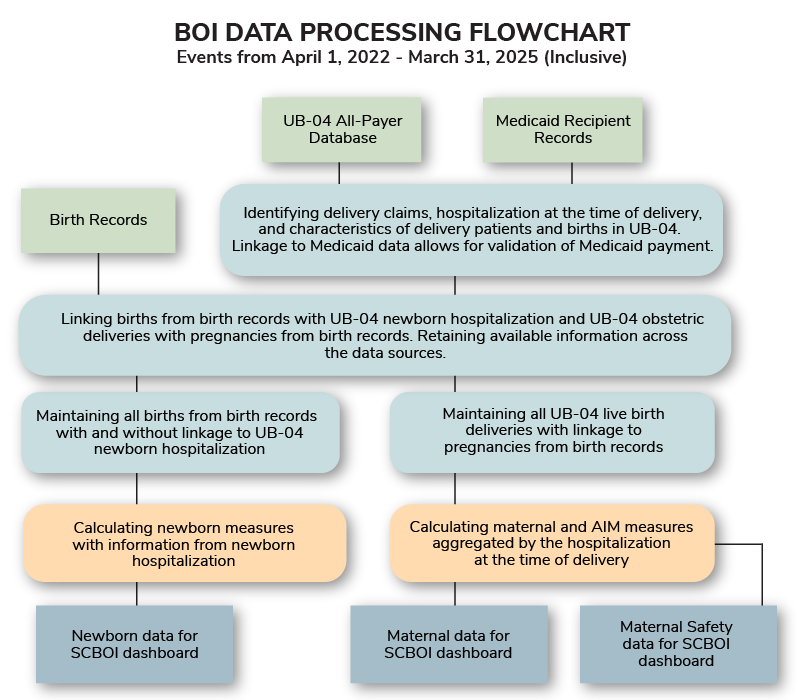
Maternal and newborn data were inclusive of hospitalizations from April 1, 2022, to March 31, 2025. SCRFA pulled all data records as of October 07, 2025. These data were restricted to only deliveries and births occurring in SC birthing facilities (i.e., data for births and deliveries among SC residents occurring outside the state of SC, at home, or in a freestanding birthing center were not included).
The maternal and newborn data were derived from three sources:
South Carolina Revenue and Fiscal Affairs Office, Health and Demographics, all-payer uniform billing data for inpatient discharges (UB-04)To maximize information, this report links birth and pregnancy data from birth records to UB-04 delivery and newborn hospitalization records.
The Joint Commission PC-02 measure does not require this linkage of obstetric hospital events with vital statistics, as some states are not set up for this level of data sharing. Linking newborn and delivery patient's UB-04 hospital data with birth records allows maximum use of the available data for newborn and maternal measures with improved accuracy of results.
What do these SCBOI data represent?
The data reflect point-in-time UB-04 data provided by individual hospitals to the SC Revenue and Fiscal Affairs Office (SCRFA) as of October 07, 2025. They may differ from a review of internal hospital medical records.
Notes: All data presented for Q1 2025 are preliminary. Outcomes presented from Q2 2022 to Q2 2023 occurred during the COVID-19 pandemic emergency; caution should be taken when comparing these rates to other quarters. Due to missing data linkages, the percentage of Medicaid may be higher than reported.
What accounts for differences in denominators?
The number of births and maternal deliveries used to calculate each maternal and newborn measure or characteristic may vary due to missing data and/or measure restrictions. Newborn measures were per neonate live birth from birth records with or without linkage to a UB-04 newborn hospitalization. The maternal delivery characteristics and labor and delivery measures were per UB-04 deliveries with linkage to a live birth from birth records. For the maternal safety measures, linkage to live birth from birth records was not required. One delivery was counted regardless of plurality.
How were demographic data determined?
Maternal demographics, such as maternal age and residence, were as of the day of delivery.
What does it mean when there is no data for a measure?
A value of zero percent (0.00%) may indicate zero births in the quarter matching the measure criteria, or an actual value of zero for a specific table result. For additional interpretation, refer to the numerators and denominators.
What measure and hospital definitions were used in this report?
The most recent definitions for newborn and maternal measures were used and applied across all time periods. Hospital data in this report reflect naming, perinatal levels, mergers, and closures identified by SCDPH as of September 2025.
How are unknown and missing data treated?
For purposes of visual presentation, Unknown and Missing values are not presented in the portal. These data are, however, included in statewide and hospital totals. Therefore, subtotals in charts may not add to 100%.